Diabetes mellitus
Diabetes mellitus: is a condition in which the body either does not produce enough, or does not properly respond to, insulin, a hormone produced in the pancreas. Insulin enables cells to absorb glucose in order to turn it into energy. In diabetes, the body either fails to properly respond to its own insulin, does not make enough insulin, or both. This causes glucose to accumulate in the blood, often leading to various complications.
what causes diabetes?
Many types of diabetes are recognized: The principal three are:
- Type 1: Results from the body's failure to produce insulin. It is estimated that 5-10% of Americans who are diagnosed with diabetes have type 1 diabetes. Presently almost all persons with type 1 diabetes must take insulin injections.
diabetes type 1
•
Type 2: Results from Insulin resistance, a condition in which cells fail to use insulin properly, sometimes combined with relative insulin deficiency. Most Americans who are diagnosed with diabetes have type 2 diabetes. Many people destined to develop type 2 diabetes spend many years in a state of Pre-diabetes: Termed "America's largest healthcare epidemic, 10-11, pre-diabetes indicates a condition that occurs when a person's blood glucose levels are higher than normal but not high enough for a diagnosis of type 2 diabetes. As of 2009 there are 57 million Americans who have pre-diabetes.
diabetes type 2
- Gestational diabetes: Pregnant women who have never had diabetes before but who have high blood sugar (glucose) levels during pregnancy are said to have gestational diabetes. Gestational diabetes affects about 4% of all pregnant women. It may precede development of type 2 (or rarely type 1).
gestational diabetes
- Many other forms of diabetes mellitus are categorized separately from these. Examples include congenital diabetes due to genetic defects of insulin secretion, cystic fibrosis-related diabetes, steroid diabetes induced by high doses of glucocorticoids, and several forms of monogenic diabetes.
All forms of diabetes have been treatable since insulin became medically available in 1921, but there is no cure for the common types except a pancreas transplant, although gestational diabetes usually resolves after delivery. Diabetes and its treatments can cause many complications. Acute complications including hypoglycemia, diabetic ketoacidosis, or nonketotic hyperosmolar coma may occur if the disease is not adequately controlled. Serious long-term complications include cardiovascular disease, chronic renal failure, retinal damage, which can lead to blindness, several types of nerve damage, and microvascular damage, which may cause erectile dysfunction and poor wound healing. Poor healing of wounds, particularly of the feet, can lead to gangrene, possibly requiring amputation. Adequate treatment of diabetes, as well as increased emphasis on blood pressure control and lifestyle factors such as not smoking and maintaining a healthy body weight, may improve the risk profile of most of the chronic complications. In the developed world, diabetes is the most significant cause of adult blindness in the non-elderly and the leading cause of non-traumatic amputation in adults, and diabetic nephropathy is the main illness requiring renal dialysis in the United States.
Classification
The term diabetes, without qualification, usually refers to diabetes mellitus, which roughly translates to excessive sweet urine (known as "glycosuria") but there are several rarer conditions also named diabetes. The most common of these is diabetes insipidus in which large amounts of urine are produced (polyuria), which is not sweet (insipidus meaning "without taste" in Latin); it can be caused either by kidney (nephrogenic DI) or pituitary gland (central DI) damage. It is a noninfectious disease. Among the body systems affected by Diabetes mellitus are the nervous, digestive, circulatory, endocrine and urinary systems, but all body systems are in some way affected.
The term "type 1 diabetes" has universally replaced several former terms, including childhood-onset diabetes, juvenile diabetes, and insulin-dependent diabetes mellitus (IDDM). Likewise, the term "type 2 diabetes" has replaced several former terms, including adult-onset diabetes, obesity-related diabetes, and non-insulin-dependent diabetes mellitus (NIDDM). Beyond these two types, there is no agreed-upon standard nomenclature. Various sources have defined "type 3 diabetes" as, among others, gestational diabetes insulin-resistant type 1 diabetes (or "double diabetes"), type 2 diabetes which has progressed to require injected insulin, and latent autoimmune diabetes of adults (or LADA or "type 1.5" diabetes.)
Type 1 diabetes
Type 1 diabetes mellitus is characterized by loss of the insulin-producing beta cells of the islets of Langerhans in the pancreas leading to a deficiency of insulin. This type of diabetes can be further classified as immune-mediated or idiopathic. The majority of type 1 diabetes is of the immune-mediated nature, where beta cell loss is a T-cell mediated autoimmune attack. There is no known preventive measure which can be taken against type 1 diabetes, which contain approximately 10% of diabetes mellitus cases in North America and Europe (though this varies by geographical location). Most affected people are otherwise healthy and of a healthy weight when onset occurs. Sensitivity and responsiveness to insulin are usually normal, especially in the early stages. Type 1 diabetes can affect children or adults but was traditionally termed "juvenile diabetes" because it represents a majority of the diabetes cases in children.
The principal treatment of type 1 diabetes, even in its earliest stages, is the delivery of artificial insulin via injection combined with careful monitoring of blood glucose levels using blood testing monitors. Without insulin, diabetic ketoacidosis often develops which may result in coma or death. Treatment emphasis is now also placed on lifestyle adjustments (diet and exercise) though these cannot reverse the progress of the disease. Apart from the common subcutaneous injections, it is also possible to deliver insulin by a pump, which allows continuous infusion of insulin 24 hours a day at preset levels, and the ability to program doses (a bolus) of insulin as needed at meal times. An inhaled form of insulin was approved by the FDA in January 2006, although it was discontinued for business reasons in October 2007. Non-insulin treatments, such as monoclonal antibodies and stem-cell based therapies, are effective in animal models but have not yet completed clinical trials in humans.
Type 1 treatment must be continued indefinitely in essentially all cases. The longest surviving Type I diabetes patient is Gladys Dull, who has lived with the condition for over 83 years. Treatment need not significantly impair normal activities, if sufficient patient training, awareness, appropriate care, discipline in testing and dosing of insulin is taken. However, treatment is burdensome for patients; insulin is replaced in a non-physiological manner, and this approach is therefore far from ideal. The average glucose level for the type 1 patient should be as close to normal (80–120 mg/dl, 4–6 mmol/L) as is safely possible. Some physicians suggest up to 140–150 mg/dl (7-7.5 mmol/L) for those having trouble with lower values, such as frequent hypoglycemic events. Values above 400 mg/dl (20 mmol/L) are sometimes accompanied by discomfort and frequent urination leading to dehydration. Values above 600 mg/dl (30 mmol/L) usually require medical treatment and may lead to ketoacidosis, although they are not immediately life-threatening. However, low levels of blood glucose, called hypoglycemia, may lead to seizures or episodes of unconsciousness and absolutely must be treated immediately, via emergency high-glucose gel placed in the patient's mouth, intravenous administration of dextrose, or an injection of glucagon.
Type 2 diabetes
Pathophysiology
Type 2 diabetes mellitus is characterized differently and is due to insulin resistance or reduced insulin sensitivity, combined with relatively reduced insulin secretion which in some cases becomes absolute. The defective responsiveness of body tissues to insulin almost certainly involves the insulin receptor in cell membranes. However, the specific defects are not known. Diabetes mellitus due to a known specific defect are classified separately. Type 2 diabetes is the most common type.
In the early stage of type 2 diabetes, the predominant abnormality is reduced insulin sensitivity, characterized by elevated levels of insulin in the blood. At this stage hyperglycemia can be reversed by a variety of measures and medications that improve insulin sensitivity or reduce glucose production by the liver. As the disease progresses, the impairment of insulin secretion worsens, and therapeutic replacement of insulin often becomes necessary.
There are numerous theories as to the exact cause and mechanism in type 2 diabetes. Central obesity (fat concentrated around the waist in relation to abdominal organs, but not subcutaneous fat) is known to predispose individuals to insulin resistance. Abdominal fat is especially active hormonally, secreting a group of hormones called adipokines that may possibly impair glucose tolerance. Obesity is found in approximately 55% of patients diagnosed with type 2 diabetes Other factors include aging (about 20% of elderly patients in North America have diabetes) and family history (type 2 is much more common in those with close relatives who have had it). In the last decade, type 2 diabetes has increasingly begun to affect children and adolescents, probably in connection with the increased prevalence of childhood obesity seen in recent decades in some places Environmental exposures may contribute to recent increases in the rate of type 2 diabetes. A positive correlation has been found between the concentration in the urine of bisphenol A, a constituent of polycarbonate plastic from some producers, and the incidence of type 2 diabetes.
Type 2 diabetes may go unnoticed for years because visible symptoms are typically mild, non-existent or sporadic, and usually there are no ketoacidotic episodes. However, severe long-term complications can result from unnoticed type 2 diabetes, including renal failure due to diabetic nephropathy, vascular disease (including coronary artery disease), vision damage due to diabetic retinopathy, loss of sensation or pain due to diabetic neuropathy, liver damage from non-alcoholic steatohepatitis and heart failure from diabetic cardiomyopathy.
Studies have suggested show that hormones like cortisol and possibly testosterone play a crucial role in the sugar absorption and in the insulin resistance It has been suggested that subclinical Cushing's syndrome (cortisol excess) is associated with diabetes mellitus type 2. The percentage of sublinical Cushing's syndrome on diabetic population seems to be about 9%, but it also seems that the real percentage is higher than previously believed. Diabetic patients with a pituitary microadenoma can significantly improve insulin sensitivity and glucose tolerance by transsphenoidal surgery, because the remotion of microadenomas can decrease ACTH and cortisol levels
Hypogonadism is often associated with cortisol excess, and testosterone deficiency is also associated with diabetes mellitus type 2, even if the exact mechanism by which testosterone improve insulin resistance is still not known.
Treatment
Type 2 diabetes is usually first treated by increasing physical activity, decreasing saturated fat and carbohydrate intake, and losing weight. These can restore insulin sensitivity even when the weight loss is modest, for example around 5 kg (10 to 15 lb), most especially when it is in abdominal fat deposits. It is sometimes possible to achieve long-term, satisfactory glucose control with these measures alone. However, the underlying tendency to insulin resistance is not lost, and so attention to diet, exercise, and weight loss must continue. The usual next step, if necessary, is treatment with oral antidiabetic drugs. Insulin production is initially only moderately impaired in type 2 diabetes, so oral medication (often used in various combinations) can be used to improve insulin production (e.g., sulfonylureas), to regulate inappropriate release of glucose by the liver and attenuate insulin resistance to some extent (e.g., metformin), and to substantially attenuate insulin resistance (e.g., thiazolidinediones). According to one study, overweight patients treated with metformin compared with diet alone, had relative risk reductions of 32% for any diabetes endpoint, 42% for diabetes related death and 36% for all cause mortality and stroke Oral medication may eventually fail due to further impairment of beta cell insulin secretion. At this point, insulin therapy is necessary to maintain normal or near normal glucose levels.
Gestational diabetes
Gestational diabetes mellitus (GDM) resembles type 2 diabetes in several respects, involving a combination of relatively inadequate insulin secretion and responsiveness. It occurs in about 2%–5% of all pregnancies and may improve or disappear after delivery. Gestational diabetes is fully treatable but requires careful medical supervision throughout the pregnancy. About 20%–50% of affected women develop type 2 diabetes later in life.
Even though it may be transient, untreated gestational diabetes can damage the health of the fetus or mother. Risks to the baby include macrosomia (high birth weight), congenital cardiac and central nervous system anomalies, and skeletal muscle malformations. Increased fetal insulin may inhibit fetal surfactant production and cause respiratory distress syndrome. Hyperbilirubinemia may result from red blood cell destruction. In severe cases, perinatal death may occur, most commonly as a result of poor placental perfusion due to vascular impairment. Induction may be indicated with decreased placental function. A cesarean section may be performed if there is marked fetal distress or an increased risk of injury associated with macrosomia, such as shoulder dystocia.
A 2008 study completed in the U.S. found that more American women are entering pregnancy with preexisting diabetes. In fact the rate of diabetes in expectant mothers has more than doubled in the past 6 years. This is particularly problematic as diabetes raises the risk of complications during pregnancy, as well as increasing the potential that the children of diabetic mothers will also become diabetic in the future.
How to Treat Gestational Diabetes
Other types
Most cases of diabetes mellitus fall into the two broad etiologic categories of type 1 or type 2 diabetes. However, many types of diabetes mellitus have more specific known causes, and thus fall into more specific categories. As more research is done into diabetes, many patients who were previously diagnosed as type 1 or type 2 diabetes will have their condition reclassified.
Some cases of diabetes are caused by the body's tissue receptors not responding to insulin (even when insulin levels are normal, which is what separates it from type 2 diabetes); this form is very uncommon. Genetic mutations (autosomal or mitochondrial) can lead to defects in beta cell function. Abnormal insulin action may also have been genetically determined in some cases. Any disease that causes extensive damage to the pancreas may lead to diabetes (for example, chronic pancreatitis and cystic fibrosis). Diseases associated with excessive secretion of insulin-antagonistic hormones can cause diabetes (which is typically resolved once the hormone excess is removed). Many drugs impair insulin secretion and some toxins damage pancreatic beta cells. The ICD-10 (1992) diagnostic entity, malnutrition-related diabetes mellitus (MRDM or MMDM, ICD-10 code E12), was deprecated by the World Health Organization when the current taxonomy was introduced in 1999.
Signs and symptoms
The classical symptoms are polyuria and polydipsia which are, respectively, frequent urination and increased thirst and consequent increased fluid intake. Symptoms may develop quite rapidly (weeks or months) in type 1 diabetes, particularly in children. However, in type 2 diabetes symptoms usually develop much more slowly and may be subtle or completely absent. Type 1 diabetes may also cause a rapid yet significant weight loss (despite normal or even increased eating) and irreducible mental fatigue. All of these symptoms except weight loss can also manifest in type 2 diabetes in patients whose diabetes is poorly controlled, although unexplained weight loss may be experienced at the onset of the disease. Final diagnosis is made by measuring the blood glucose concentration.
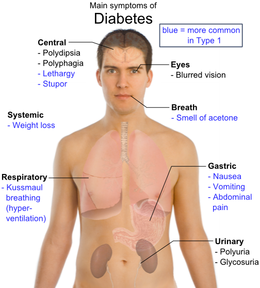
Overview of the most significant symptoms of diabetes.
When the glucose concentration in the blood is raised beyond its renal threshold (about 10 mmol/L, although this may be altered in certain conditions, such as pregnancy), reabsorption of glucose in the proximal renal tubuli is incomplete, and part of the glucose remains in the urine (glycosuria). This increases the osmotic pressure of the urine and inhibits reabsorption of water by the kidney, resulting in increased urine production (polyuria) and increased fluid loss. Lost blood volume will be replaced osmotically from water held in body cells and other body compartments, causing dehydration and increased thirst.
Prolonged high blood glucose causes glucose absorption, which leads to changes in the shape of the lenses of the eyes, resulting in vision changes; sustained sensible glucose control usually returns the lens to its original shape. Blurred vision is a common complaint leading to a diabetes diagnosis; type 1 should always be suspected in cases of rapid vision change, whereas with type 2 change is generally more gradual, but should still be suspected.
diabetes symptoms
Patients (usually with type 1 diabetes) may also initially present with diabetic ketoacidosis (DKA), an extreme state of metabolic dysregulation characterized by the smell of acetone on the patient's breath; a rapid, deep breathing known as Kussmaul breathing; polyuria; nausea; vomiting and abdominal pain; and any of many altered states of consciousness or arousal (such as hostility and mania or, equally, confusion and lethargy). In severe DKA, coma may follow, progressing to death. Diabetic ketoacidosis is a medical emergency and requires immediate hospitalization.
A rarer but equally severe possibility is hyperosmolar nonketotic state, which is more common in type 2 diabetes and is mainly the result of dehydration due to loss of body water. Often, the patient has been drinking extreme amounts of sugar-containing drinks, leading to a vicious circle in regard to the water loss.
Genetics
Both type 1 and type 2 diabetes are at least partly inherited. Type 1 diabetes appears to be triggered by some (mainly viral) infections, with some evidence pointing at Coxsackie B4 virus. There is a genetic element in individual susceptibility to some of these triggers which has been traced to particular HLA genotypes (i.e., the genetic "self" identifiers relied upon by the immune system). However, even in those who have inherited the susceptibility, type 1 diabetes mellitus seems to require an environmental trigger.
There is a stronger inheritance pattern for type 2 diabetes. Those with first-degree relatives with type 2 have a much higher risk of developing type 2, increasing with the number of those relatives. Concordance among monozygotic twins is close to 100%, and about 25% of those with the disease have a family history of diabetes. Genes significantly associated with developing type 2 diabetes, include TCF7L2, PPARG, FTO, KCNJ11, NOTCH2, WFS1, CDKAL1, IGF2BP2, SLC30A8, JAZF1, and HHEX. KCNJ11 (potassium inwardly rectifying channel, subfamily J, member 11), encodes the islet ATP-sensitive potassium channel Kir6.2, and TCF7L2 (transcription factor 7–like 2) regulates proglucagon gene expression and thus the production of glucagon-like peptide-1. Moreover, obesity (which is an independent risk factor for type 2 diabetes) is strongly inherited.
Monogenic forms, e.g., MODY, constitute 1-5 % of all cases.
Various hereditary conditions may feature diabetes, for example myotonic dystrophy and Friedreich's ataxia. Wolfram's syndrome is an autosomal recessive neurodegenerative disorder that first becomes evident in childhood. It consists of diabetes insipidus, diabetes mellitus, optic atrophy, and deafness, hence the acronym DIDMOAD.
Gene expression promoted by a diet of fat and glucose as well as high levels of inflammation related cytokines found in the obese results in cells that "produce fewer and smaller mitochondria than is normal," and are thus prone to insulin resistance.
Pathophysiology
Insulin is the principal hormone that regulates uptake of glucose from the blood into most cells (primarily muscle and fat cells, but not central nervous system cells). Therefore deficiency of insulin or the insensitivity of its receptors plays a central role in all forms of diabetes mellitus.
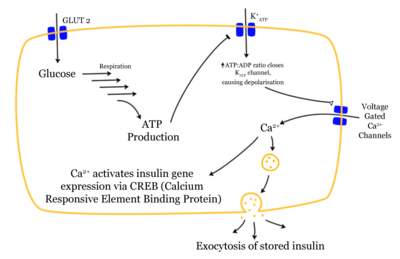
Mechanism of insulin release in normal pancreatic beta cells. Insulin production is more or less constant within the beta cells, irrespective of blood glucose levels. It is stored within vacuoles pending release, via exocytosis, which is primarily triggered by food, chiefly food containing absorbable glucose. The chief trigger is a rise in blood glucose levels after eating
Most of the carbohydrates in food are converted within a few hours to the monosaccharide glucose, the principal carbohydrate found in blood and used by the body as fuel. The most significant exceptions are fructose, most disaccharides (except sucrose and in some people lactose), and all more complex polysaccharides, with the outstanding exception of starch. Insulin is released into the blood by beta cells (β-cells), found in the Islets of Langerhans in the pancreas, in response to rising levels of blood glucose, typically after eating. Insulin is used by about two-thirds of the body's cells to absorb glucose from the blood for use as fuel, for conversion to other needed molecules, or for storage.
Insulin is also the principal control signal for conversion of glucose to glycogen for internal storage in liver and muscle cells. Lowered glucose levels result both in the reduced release of insulin from the beta cells and in the reverse conversion of glycogen to glucose when glucose levels fall. This is mainly controlled by the hormone glucagon which acts in an opposite manner to insulin. Glucose thus recovered by the liver re-enters the bloodstream; muscle cells lack the necessary export mechanism.
Higher insulin levels increase some anabolic ("building up") processes such as cell growth and duplication, protein synthesis, and fat storage. Insulin (or its lack) is the principal signal in converting many of the bidirectional processes of metabolism from a catabolic to an anabolic direction, and vice versa. In particular, a low insulin level is the trigger for entering or leaving ketosis (the fat burning metabolic phase).
If the amount of insulin available is insufficient, if cells respond poorly to the effects of insulin (insulin insensitivity or resistance), or if the insulin itself is defective, then glucose will not be absorbed properly by those body cells that require it nor will it be stored appropriately in the liver and muscles. The net effect is persistent high levels of blood glucose, poor protein synthesis, and other metabolic derangements, such as acidosis.
Diagnosis
The diagnosis of type 1 diabetes, and many cases of type 2, is usually prompted by recent-onset symptoms of excessive urination (polyuria) and excessive thirst (polydipsia), often accompanied by weight loss. These symptoms typically worsen over days to weeks; about a quarter of people with new type 1 diabetes have developed some degree of diabetic ketoacidosis (a type of metabolic acidosis which is caused by high concentrations of ketone bodies, formed by the breakdown of fatty acids and the deamination of amino acids) by the time the diabetes is recognized. The diagnosis of other types of diabetes is usually made in other ways. These include ordinary health screening; detection of hyperglycemia during other medical investigations; and secondary symptoms such as vision changes or unexplainable fatigue. Diabetes is often detected when a person suffers a problem that is frequently caused by diabetes, such as a heart attack, stroke, neuropathy, poor wound healing or a foot ulcer, certain eye problems, certain fungal infections, or delivering a baby with macrosomia or hypoglycemia.
Diabetes mellitus is characterized by recurrent or persistent hyperglycemia, and is diagnosed by demonstrating any one of the following:
- Fasting plasma glucose level at or above 126 mg/dL (7.0 mmol/L).
- Plasma glucose at or above 200 mg/dL (11.1 mmol/L) two hours after a 75 g oral glucose load as in a glucose tolerance test.
- Symptoms of hyperglycemia and casual plasma glucose at or above 200 mg/dL (11.1 mmol/L).
A positive result, in the absence of unequivocal hyperglycemia, should be confirmed by a repeat of any of the above-listed methods on a different day. Most physicians prefer to measure a fasting glucose level because of the ease of measurement and the considerable time commitment of formal glucose tolerance testing, which takes two hours to complete and offers no prognostic advantage over the fasting test. According to the current definition, two fasting glucose measurements above 126 mg/dL (7.0 mmol/L) is considered diagnostic for diabetes mellitus.
Patients with fasting glucose levels from 100 to 125 mg/dL (6.1 and 7.0 mmol/L) are considered to have impaired fasting glucose. Patients with plasma glucose at or above 140 mg/dL or 7.8 mmol/L, but not over 200, two hours after a 75 g oral glucose load are considered to have impaired glucose tolerance. Of these two pre-diabetic states, the latter in particular is a major risk factor for progression to full-blown diabetes mellitus as well as cardiovascular disease.
While not used for diagnosis, an elevated level of glucose irreversibly bound to hemoglobin (termed glycated hemoglobin or HbA1c) of 6.0% or higher (the 2003 revised U.S. standard) is considered abnormal by most labs; HbA1c is primarily used as a treatment-tracking test reflecting average blood glucose levels over the preceding 90 days (approximately) which is the average lifetime of red blood cells which contain hemoglobin in most patients. However, some physicians may order this test at the time of diagnosis to track changes over time. The current recommended goal for HbA1c in patients with diabetes is 6.5%.
Screening
Diabetes screening is recommended for many people at various stages of life, and for those with any of several risk factors. The screening test varies according to circumstances and local policy, and may be a random blood glucose test, a fasting blood glucose test, a blood glucose test two hours after 75 g of glucose, or an even more formal glucose tolerance test. Many healthcare providers recommend universal screening for adults at age 40 or 50, and often periodically thereafter. Earlier screening is typically recommended for those with risk factors such as obesity, family history of diabetes, high-risk ethnicity (Hispanic, Native American, Afro-Caribbean, Pacific Islander, or Maori).
Many medical conditions are associated with diabetes and warrant screening. A partial list includes: subclinical Cushing's syndrome, testosterone deficiency, high blood pressure, elevated cholesterol levels, coronary artery disease, past gestational diabetes, polycystic ovary syndrome, chronic pancreatitis, fatty liver, hemochromatosis, cystic fibrosis, several mitochondrial neuropathies and myopathies, myotonic dystrophy, Friedreich's ataxia, some of the inherited forms of neonatal hyperinsulinism. The risk of diabetes is higher with chronic use of several medications, including high-dose glucocorticoids, some chemotherapy agents (especially L-asparaginase), as well as some of the antipsychotics and mood stabilizers (especially phenothiazines and some atypical antipsychotics).
People with a confirmed diagnosis of diabetes are tested routinely for complications. This includes yearly urine testing for microalbuminuria and examination of the retina of the eye for retinopathy.
Prevention
Type 1 diabetes risk is known to depend upon a genetic predisposition based on HLA types (particularly types DR3 and DR4), an unknown environmental trigger (suspected to be an infection, although none has proven definitive in all cases), and an uncontrolled autoimmune response that attacks the insulin producing beta cells. Some research has suggested that breastfeeding decreased the risk in later life; various other nutritional risk factors are being studied, but no firm evidence has been found Giving children 2000 IU of Vitamin D during their first year of life is associated with reduced risk of type 1 diabetes, though the causal relationship is obscure
Children with antibodies to beta cell proteins (ie at early stages of an immune reaction to them) but no overt diabetes, and treated with vitamin B-3 (niacin), had less than half the diabetes onset incidence in a 7-year time span as did the general population, and an even lower incidence relative to those with antibodies as above, but who received no vitamin B3.
Type 2 diabetes risk can be reduced in many cases by making changes in diet and increasing physical activity. The American Diabetes Association (ADA) recommends maintaining a healthy weight, getting at least 2½ hours of exercise per week (several brisk sustained walks appear sufficient), having a modest fat intake, and eating sufficient fiber (e.g., from whole grains). The ADA does not recommend alcohol consumption as a preventive, but it is interesting to note that moderate alcohol intake may reduce the risk (though heavy consumption absolutely and clearly increases damage to bodily systems significantly); a similarly confused connection between low dose alcohol consumption and heart disease is termed the French Paradox.
There is inadequate evidence that eating foods of low glycemic index is clinically helpful despite recommendations and suggested diets emphasizing this approach.
diabetes prevention
Diets that are very low in saturated fats reduce the risk of becoming insulin resistant and diabetic. Study group participants whose "physical activity level and dietary, smoking, and alcohol habits were all in the low-risk group had an 82% lower incidence of diabetes." In another study of dietary practice and incidence of diabetes, "foods rich in vegetable oils, including non-hydrogenated margarines, nuts, and seeds, should replace foods rich in saturated fats from meats and fat-rich dairy products. Consumption of partially hydrogenated fats should be minimized."
There are numerous studies which suggest connections between some aspects of Type II diabetes with ingestion of certain foods or with some drugs. Some studies have shown delayed progression to diabetes in predisposed patients through prophylactic use of metformin, rosiglitazone, or valsartan In patients on hydroxychloroquine for rheumatoid arthritis, incidence of diabetes was reduced by 77% though causal mechanisms are unclear. Breastfeeding may also be associated with the prevention of type 2 of the disease in mothers. Clear evidence for these and any of many other connections between foods and supplements and diabetes is sparse to date; none, despite secondary claims for (or against), is sufficiently well established to justify as a standard clinical approach.
Treatment and management
Diabetes mellitus is currently a chronic disease with no cure. Medical emphasis must necessarily be on managing/avoiding possible short-term as well as long-term diabetes-related problems. There is an exceptionally important role for patient education, dietetic support, sensible exercise, self monitoring of blood glucose, with the goal of keeping both short-term and long-term blood glucose levels within acceptable bounds. Careful control is needed to reduce the risk of long term complications. This is theoretically achievable with combinations of diet, exercise and weight loss (type 2), various oral diabetic drugs (type 2 only), and insulin use (type 1 and for type 2 not responding to oral medications, mostly those with extended duration diabetes). In addition, given the associated higher risks of cardiovascular disease, lifestyle modifications should be undertaken to control blood pressure and cholesterol by exercising more, smoking less or ideally not at all, consuming an appropriate diet, wearing diabetic socks, wearing diabetic shoes, and if necessary, taking any of several drugs to reduce blood pressure. Many type 1 treatments include combination use of regular or NPH insulin, and/or synthetic insulin analogs (e.g., Humalog, Novolog or Apidra) in combinations such as Lantus/Levemir and Humalog, Novolog or Apidra. Another type 1 treatment option is the use of the insulin pump (e.g., from Deltec Cozmo, Animas, Medtronic Minimed, Insulet Omnipod, or ACCU-CHEK). A blood lancet is used to pierce the skin (typically of a finger), in order to draw blood to test it for sugar levels.
managing diabetes long-term
In countries using a general practitioner system, such as the United Kingdom, care may take place mainly outside hospitals, with hospital-based specialist care used only in case of complications, difficult blood sugar control, or research projects. In other circumstances, general practitioners and specialists share care of a patient in a team approach. Optometrists, podiatrists/chiropodists, dietitians, physiotherapists, nursing specialists (e.g., DSNs (Diabetic Specialist Nurse)), nurse practitioners, or Certified Diabetes Educators, may jointly provide multidisciplinary expertise. In countries where patients must provide for their own health care (e.g in the US, and in much of the undeveloped world), the impact of out-of-pocket costs of adequate diabetic care can be very high. In addition to the medications and supplies needed, patients are often advised to receive regular consultation from a physician (e.g., at least every three to six months) although research is underway to develop artificial intelligence systems which may reduce the frequency of such visits. Oral administration of aloe vera might be a useful adjunct for lowering blood glucose in diabetic patients as well as for reducing blood lipid levels in patients with hyperlipidaemia. Ten controlled clinical trials were found to reach that conclusion in four independent literature searches. However, caveats reported in each study led the researchers to conclude that aloe vera's clinical effectiveness was not yet sufficiently defined in 1999.
Peer support links people living with diabetes. Within peer support, people with a common illness share knowledge and experience that others, including many health workers, do not have. Peer support is frequent, ongoing, accessible and flexible and can take many forms—phone calls, text messaging, group meetings, home visits, and even grocery shopping. It complements and enhances other health care services by creating the emotional, social and practical assistance necessary for managing disease and staying healthy.
diabetes treatment and cure
Cure
Cures for type 1 diabetes
There is no practical cure, at this time, for type 1 diabetes. The fact that type 1 diabetes is due to the failure of one of the cell types of a single organ with a relatively simple function (i.e. the failure of the beta cells in the Islets of Langerhans) has led to the study of several possible schemes to cure this form of diabetes mostly by replacing the pancreas or just the beta cells. Only those type 1 diabetics who have received either a pancreas or a kidney-pancreas transplant (often when they have developed diabetic kidney disease (ie, nephropathy) and become insulin-independent) may now be considered "cured" from their diabetes. A simultaneous pancreas-kidney transplant is a promising solution, showing similar or improved survival rates over a kidney transplant alone. Still, they generally remain on long-term immunosuppressive drugs and there is a possibility that the immune system will mount a host versus graft response against the transplanted organ
Transplants of exogenous beta cells have been performed experimentally in both mice and humans, but this measure is not yet practical in regular clinical practice partly due to the limited number of beta cell donors. Thus far, like any such transplant, it has provoked an immune reaction and long-term immunosuppressive drugs have been needed to protect the transplanted tissue. An alternative technique has been proposed to place transplanted beta cells in a semi-permeable container, isolating and protecting them from the immune system. Stem cell research has also been suggested as a potential avenue for a cure since it may permit regrowth of Islet cells which are genetically part of the treated individual, thus perhaps eliminating the need for immuno-suppressants.
This new method autologous nonmyeloablative hematopoietic stem cell transplantation was developed by a research team composed by Brazilian and American scientists (Dr. Julio Voltarelli, Dr. Carlos Eduardo Couri, Dr Richard Burt, and colleagues) and it was the first study to use stem cell therapy in human diabetes mellitus. This was initially tested in mice and in 2007 there was the first publication of stem cell therapy to treat this form of diabetes. Until 2009, there was 23 patients included and followed for a mean period of 29.8 months (ranging from 7 to 58 months). In the trial, severe immunosuppresion with high doses of cyclophosphamide and anti-thymocyte globulin is used with the aim of "turning off" the immunologic system", and then autologous hematopoietic stem cells are reinfused to regenerate a new one. In summary it is a kind of "immunologic reset" that blocks the autoimmune attack against residual pancreatic insulin-producing cells. Until December 2009, 12 patients remained continuously insulin-free for periods raging from 14 to 52 months and 8 patients became transiently insulin-free for periods ranging from 6 to 47 months. Of these last 8 patients, 2 became insulin-free again after the use of sitagliptin, a DPP-4 inhibitor approved only to treat type 2 diabetic patients and this is also the first study to document the use and complete insulin-independendce in humans with type 1 diabetes with this medication. In parallel with insulin suspension, indirect measures of endogenous insulin secretion revealed thate it significantly increased in the whole group of patients, regardless the need of daily exogenous insulin use.
Microscopic or nanotechnological approaches are under investigation as well, in one proposed case with implanted stores of insulin metered out by a rapid response valve sensitive to blood glucose levels. At least two approaches have been demonstrated in vitro. These are, in some sense, closed-loop insulin pumps.
Cures for type 2 diabetes
Type 2 diabetes is usually first treated by increasing physical activity, and eliminating saturated fat and reducing sugar and carbohydrate intake with a goal of losing weight. These can restore insulin sensitivity even when the weight loss is modest, for example around 5 kg (10 to 15 lb), most especially when it is in abdominal fat deposits. Diets that are very low in saturated fats can reverse insulin resistance
Testosterone replacement therapy can improve glucose tolerance and insulin sensitivity in diabetic hypogonadal men. The mechanisms by which testosterone decreases insulin resistance is under study. Moreover testosterone has a protective effect on pancreatic beta cells, which is possibly exerted by androgen-receptor-mediated mechanisms and influence of inflammatory cytokines.
Recently it has been shown that a type of gastric bypass surgery can normalize blood glucose levels in 80-100% of severely obese patients with diabetes. The precise causal mechanisms are being intensively researched; its results are not simply attributable to weight loss, as the improvement in blood sugars precedes any change in body mass. This approach may become a standard treatment for some people with type 2 diabetes in the relatively near future. This surgery has the additional benefit of reducing the death rate from all causes by up to 40% in severely obese people. A small number of normal to moderately obese patients with type 2 diabetes have successfully undergone similar operations.
Complications and prognosis
Patient education, understanding, and participation is vital since the complications of diabetes are far less common and less severe in people who have well-controlled blood sugar levels Wider health problems accelerate the deleterious effects of diabetes. These include smoking, elevated cholesterol levels, obesity, high blood pressure, and lack of regular exercise. According to one study, women with high blood pressure (hypertension) were three times more likely to develop type 2 diabetes as compared with women with optimal BP after adjusting for various factors such as age, ethnicity, smoking, alcohol intake, body mass index (BMI), exercise, family history of diabetes, etc. The study was conducted by researchers from the Brigham and Women’s Hospital, Harvard Medical School and the Harvard School of Public Health, USA, who followed over 38,000 female health professionals for ten years.
Anecdotal evidence suggests that some of those with type 2 diabetes who exercise regularly, lose weight, and eat healthy diets may be able to keep some of the disease or some of the effects of the disease in 'remission.' Certainly these tips can help prevent people predisposed to type 2 diabetes and those at pre-diabetic stages from actually developing the disorder as it helps restore insulin sensitivity. However patients should talk to their doctors about this for real expectations before undertaking it (esp. to avoid hypoglycemia or other complications); few people actually seem to go into total 'remission,' but some may find they need less of their insulin medications since the body tends to have lower insulin requirements during and shortly following exercise. Regardless of whether it works that way or not for an individual, there are certainly other benefits to this healthy lifestyle for both diabetics and nondiabetics.
The way diabetes is managed changes with age. Insulin production decreases because of age-related impairment of pancreatic beta cells. Additionally, insulin resistance increases because of the loss of lean tissue and the accumulation of fat, particularly intra-abdominal fat, and the decreased tissue sensitivity to insulin. Glucose tolerance progressively declines with age, leading to a high prevalence of type 2 diabetes and postchallenge hyperglycemia in the older population Age-related glucose intolerance in humans is often accompanied by insulin resistance, but circulating insulin levels are similar to those of younger people. Treatment goals for older patients with diabetes vary with the individual, and take into account health status, as well as life expectancy, level of dependence, and willingness to adhere to a treatment regimen.
Acute complications
Diabetic ketoacidosis (DKA) is an acute and dangerous complication that is always a medical emergency. Low insulin levels cause the liver to turn to fat for fuel (ie, ketosis); ketone bodies are intermediate substrates in that metabolic sequence. This is normal when periodic, but can become a serious problem if sustained. Elevated levels of ketone bodies in the blood decrease the blood's pH, leading to DKA. On presentation at hospital, the patient in DKA is typically dehydrated, and breathing rapidly and deeply. Abdominal pain is common and may be severe. The level of consciousness is typically normal until late in the process, when lethargy may progress to coma. Ketoacidosis can easily become severe enough to cause hypotension, shock, and death. Urine analysis will reveal significant levels of ketone bodies (which have exceeded their renal threshold blood levels to appear in the urine, often before other overt symptoms). Prompt, proper treatment usually results in full recovery, though death can result from inadequate or delayed treatment, or from complications (e.g., brain edema). DKA is always a medical emergency and requires medical attention. Ketoacidosis is much more common in type 1 diabetes than type 2.
Hyperosmolar nonketotic state (HNS) is an acute complication sharing many symptoms with DKA, but an entirely different origin and different treatment. A person with very high (usually considered to be above 300 mg/dl (16 mmol/L)) blood glucose levels, water is osmotically drawn out of cells into the blood and the kidneys eventually begin to dump glucose into the urine. This results in loss of water and an increase in blood osmolarity. If fluid is not replaced (by mouth or intravenously), the osmotic effect of high glucose levels, combined with the loss of water, will eventually lead to dehydration. The body's cells become progressively dehydrated as water is taken from them and excreted. Electrolyte imbalances are also common and are always dangerous. As with DKA, urgent medical treatment is necessary, commonly beginning with fluid volume replacement. Lethargy may ultimately progress to a coma, though this is more common in type 2 diabetes than type 1.
Hypoglycemia, or abnormally low blood glucose, is an acute complication of several diabetes treatments. It is rare otherwise, either in diabetic or non-diabetic patients. The patient may become agitated, sweaty, weak, and have many symptoms of sympathetic activation of the autonomic nervous system resulting in feelings akin to dread and immobilized panic. Consciousness can be altered or even lost in extreme cases, leading to coma, seizures, or even brain damage and death. In patients with diabetes, this may be caused by several factors, such as too much or incorrectly timed insulin, too much or incorrectly timed exercise (exercise decreases insulin requirements) or not enough food (specifically glucose containing carbohydrates). The variety of interactions makes cause identification difficult in many instances.
It is more accurate to note that iatrogenic hypoglycemia is typically the result of the interplay of absolute (or relative) insulin excess and compromised glucose counterregulation in type 1 and advanced type 2 diabetes. Decrements in insulin, increments in glucagon, and, absent the latter, increments in epinephrine are the primary glucose counterregulatory factors that normally prevent or (more or less rapidly) correct hypoglycemia. In insulin-deficient diabetes (exogenous) insulin levels do not decrease as glucose levels fall, and the combination of deficient glucagon and epinephrine responses causes defective glucose counterregulation.
Furthermore, reduced sympathoadrenal responses can cause hypoglycemia unawareness. The concept of hypoglycemia-associated autonomic failure (HAAF) in diabetes posits that recent incidents of hypoglycemia causes both defective glucose counterregulation and hypoglycemia unawareness. By shifting glycemic thresholds for the sympathoadrenal (including epinephrine) and the resulting neurogenic responses to lower plasma glucose concentrations, antecedent hypoglycemia leads to a vicious cycle of recurrent hypoglycemia and further impairment of glucose counterregulation. In many cases (but not all), short-term avoidance of hypoglycemia reverses hypoglycemia unawareness in affected patients, although this is easier in theory than in clinical experience.
In most cases, hypoglycemia is treated with sugary drinks or food. In severe cases, an injection of glucagon (a hormone with effects largely opposite to those of insulin) or an intravenous infusion of dextrose is used for treatment, but usually only if the person is unconscious. In any given incident, glucagon will only work once as it uses stored liver glycogen as a glucose source; in the absence of such stores, glucagon is largely ineffective. In hospitals, intravenous dextrose is often used.
Respiratory infections
The immune response is impaired in individuals with diabetes mellitus. Cellular studies have shown that hyperglycemia both reduces the function of immune cells and increases inflammation. The vascular effects of diabetes also tend to alter lung function, all of which leads to an increase in susceptibility to respiratory infections such as pneumonia and influenza among individuals with diabetes. Several studies also show diabetes associated with a worse disease course and slower recovery from respiratory infections.
Chronic complications
Chronic elevation of blood glucose level leads to damage of blood vessels (angiopathy). The endothelial cells lining the blood vessels take in more glucose than normal, since they don't depend on insulin. They then form more surface glycoproteins than normal, and cause the basement membrane to grow thicker and weaker. In diabetes, the resulting problems are grouped under "microvascular disease" (due to damage to small blood vessels) and "macrovascular disease" (due to damage to the arteries).
However, some research challenges the theory of hyperglycemia as the cause of diabetic complications. The fact that 40% of diabetics who carefully control their blood sugar nevertheless develop neuropathy, and that some of those with good blood sugar control still develop nephropathy, requires explanation. It has been discovered that the serum of diabetics with neuropathy is toxic to nerves even if its blood sugar content is normal. Recent research suggests that in type 1 diabetics, the continuing autoimmune immune disease which initially destroyed the beta cells of the pancreas may also cause retinopathy, neuropathy, and nephropathy. One researcher has even suggested that retinopathy may be better treated by drugs to suppress the abnormal immune system of diabetics than by blood sugar control. The familial clustering of the degree and type of diabetic complications indicates that genetics may also play a role in causing complications such as diabetic retinopathy. and nephropathy Non-diabetic offspring of type 2 diabetics have been found to have increased arterial stiffness and neuropathy despite normal blood glucose levels, and elevated enzyme levels associated with diabetic renal disease have been found in non-diabetic first-degree relatives of diabetics. Even rapid tightening of blood glucose levels has been shown to worsen rather than improve diabetic complications, though it has usually been held that complications would improve over time with more normal blood sugar, provided this could be maintained. However. one study continued for 41 months found that the initial worsening of complications from improved glucose control was not followed by the expected improvement in the complications.
The damage to small blood vessels leads to a microangiopathy, which can cause one or more of the following:
- Diabetic retinopathy, growth of friable and poor-quality new blood vessels in the retina as well as macular edema (swelling of the macula), which can lead to severe vision loss or blindness. Retinal damage (from microangiopathy) makes it the most common cause of blindness among non-elderly adults in the US.
- Diabetic neuropathy, abnormal and decreased sensation, usually in a 'glove and stocking' distribution starting with the feet but potentially in other nerves, later often fingers and hands. When combined with damaged blood vessels this can lead to diabetic foot (see below). Other forms of diabetic neuropathy may present as mononeuritis or autonomic neuropathy. Diabetic amyotrophy is muscle weakness due to neuropathy.
- Diabetic nephropathy, damage to the kidney which can lead to chronic renal failure, eventually requiring dialysis. Diabetes mellitus is the most common cause of adult kidney failure worldwide in the developed world.
- Diabetic cardiomyopathy, damage to the heart, leading to diastolic dysfunction and eventually heart failure.
Macrovascular disease leads to cardiovascular disease, to which accelerated atherosclerosis is a contributor:
- Coronary artery disease, leading to angina or myocardial infarction ("heart attack")
- Stroke (mainly the ischemic type)
- Peripheral vascular disease, which contributes to intermittent claudication (exertion-related leg and foot pain) as well as diabetic foot.
- Diabetic myonecrosis ('muscle wasting')
Diabetic foot, often due to a combination of sensory neuropathy (numbness or insensitivity) and vascular damage, increases rates of skin ulcers and infection and, in serious cases, necrosis and gangrene. It is why diabetics are prone to leg and foot infections and why it takes longer for them to heal from leg and foot wounds. It is the most common cause of non-traumatic adult amputation, usually of toes and or feet, in the developed world.
Carotid artery stenosis does not occur more often in diabetes, and there appears to be a lower prevalence of abdominal aortic aneurysm. However, diabetes does cause higher morbidity, mortality and operative risks with these conditions.
Diabetic encephalopathy is the increased cognitive decline and risk of dementia observed in diabetes. Various mechanisms are proposed, including alterations to the vascular supply of the brain and the interaction of insulin with the brain itself.
Epidemiology
In 2000, according to the World Health Organization, at least 171 million people worldwide suffer from diabetes, or 2.8% of the population. Its incidence is increasing rapidly, and it is estimated that by the year 2030, this number will almost double. Diabetes mellitus occurs throughout the world, but is more common (especially type 2) in the more developed countries. The greatest increase in prevalence is, however, expected to occur in Asia and Africa, where most patients will probably be found by 2030. The increase in incidence of diabetes in developing countries follows the trend of urbanization and lifestyle changes, perhaps most importantly a "Western-style" diet. This has suggested an environmental (i.e., dietary) effect, but there is little understanding of the mechanism(s) at present, though there is much speculation, some of it most compellingly presented.
For at least 20 years, diabetes rates in North America have been increasing substantially. In 2008 there were about 24 million people with diabetes in the United States alone, from those 5.7 million people remain undiagnosed. Other 57 million people are estimated to have pre-diabetes.
The Centers for Disease Control has termed the change an epidemic. The National Diabetes Information Clearinghouse estimates that diabetes costs $132 billion in the United States alone every year. About 5%–10% of diabetes cases in North America are type 1, with the rest being type 2. The fraction of type 1 in other parts of the world differs; this is probably due to both differences in the rate of type 1 and differences in the rate of other types, most prominently type 2. Most of this difference is not currently understood. The American Diabetes Association cite the 2003 assessment of the National Center for Chronic Disease Prevention and Health Promotion (Centers for Disease Control and Prevention) that 1 in 3 Americans born after 2000 will develop diabetes in their lifetime.
According to the American Diabetes Association, approximately 18.3% (8.6 million) of Americans age 60 and older have diabetes. Diabetes mellitus prevalence increases with age, and the numbers of older persons with diabetes are expected to grow as the elderly population increases in number. The National Health and Nutrition Examination Survey (NHANES III) demonstrated that, in the population over 65 years old, 18% to 20% have diabetes, with 40% having either diabetes or its precursor form of impaired glucose tolerance.
Indigenous populations in first world countries have a higher prevalence and increasing incidence of diabetes than their corresponding non-indigenous populations. In Australia the age-standardised prevalence of self-reported diabetes in Indigenous Australians is almost 4 times that of non-indigenous Australians. Preventative community health programs such as Sugar Man (diabetes education) are showing some success in tackling this problem.
History
The term diabetes (Greek: διαβήτης, diabētēs) was coined by Aretaeus of Cappadocia. It was derived from the Greek verb διαβαίνειν, diabaínein, itself formed from the prefix dia-, "across, apart," and the verb bainein, "to walk, stand." The verb diabeinein meant "to stride, walk, or stand with legs asunder"; hence, its derivative diabētēs meant "one that straddles," or specifically "a compass, siphon." The sense "siphon" gave rise to the use of diabētēs as the name for a disease involving the discharge of excessive amounts of urine. Diabetes is first recorded in English, in the form diabete, in a medical text written around 1425. In 1675, Thomas Willis added the word mellitus, from the Latin meaning "honey", a reference to the sweet taste of the urine. This sweet taste had been noticed in urine by the ancient Greeks, Chinese, Egyptians, Indians, and Persians. In 1776, Matthew Dobson confirmed that the sweet taste was because of an excess of a kind of sugar in the urine and blood of people with diabetes.
Diabetes mellitus appears to have been a death sentence in the ancient era. Hippocrates makes no mention of it, which may indicate that he felt the disease was incurable. Aretaeus did attempt to treat it but could not give a good prognosis; he commented that "life (with diabetes) is short, disgusting and painful."
Sushruta (6th century BCE) identified diabetes and classified it as Medhumeha. He further identified it with obesity and sedentary lifestyle, advising exercises to help "cure" it. The ancient Indians tested for diabetes by observing whether ants were attracted to a person's urine, and called the ailment "sweet urine disease" (Madhumeha). The Korean, Chinese, and Japanese words for diabetes are based on the same ideographs (糖尿病) which mean "sugar urine disease".
In medieval Persia, Avicenna (980-1037) provided a detailed account on diabetes mellitus in The Canon of Medicine, "describing the abnormal appetite and the collapse of sexual functions and he documented the sweet taste of diabetic urine." Like Aretaeus before him, Avicenna recognized a primary and secondary diabetes. He also described diabetic gangrene, and treated diabetes using a mixture of lupine, trigonella (fenugreek), and zedoary seed, which produces a considerable reduction in the excretion of sugar, a treatment which is still prescribed in modern times. Avicenna also "described diabetes insipidus very precisely for the first time", though it was later Johann Peter Frank (1745-1821) who first differentiated between diabetes mellitus and diabetes insipidus.
Although diabetes has been recognized since antiquity, and treatments of various efficacy have been known in various regions since the Middle Ages, and in legend for much longer, pathogenesis of diabetes has only been understood experimentally since about 1900. The discovery of a role for the pancreas in diabetes is generally ascribed to Joseph von Mering and Oskar Minkowski, who in 1889 found that dogs whose pancreas was removed developed all the signs and symptoms of diabetes and died shortly afterwards. In 1910, Sir Edward Albert Sharpey-Schafer suggested that people with diabetes were deficient in a single chemical that was normally produced by the pancreas—he proposed calling this substance insulin, from the Latin insula, meaning island, in reference to the insulin-producing islets of Langerhans in the pancreas.
The endocrine role of the pancreas in metabolism, and indeed the existence of insulin, was not further clarified until 1921, when Sir Frederick Grant Banting and Charles Herbert Best repeated the work of Von Mering and Minkowski, and went further to demonstrate they could reverse induced diabetes in dogs by giving them an extract from the pancreatic islets of Langerhans of healthy dogs. Banting, Best, and colleagues (especially the chemist Collip) went on to purify the hormone insulin from bovine pancreases at the University of Toronto. This led to the availability of an effective treatment—insulin injections—and the first patient was treated in 1922. For this, Banting and laboratory director MacLeod received the Nobel Prize in Physiology or Medicine in 1923; both shared their Prize money with others in the team who were not recognized, in particular Best and Collip. Banting and Best made the patent available without charge and did not attempt to control commercial production. Insulin production and therapy rapidly spread around the world, largely as a result of this decision. Banting is honored by World Diabetes Day which is held on his birthday, November 14.
The distinction between what is now known as type 1 diabetes and type 2 diabetes was first clearly made by Sir Harold Percival (Harry) Himsworth, and published in January 1936.
Despite the availability of treatment, diabetes has remained a major cause of death. For instance, statistics reveal that the cause-specific mortality rate during 1927 amounted to about 47.7 per 100,000 population in Malta.
Other landmark discoveries include:
- Identification of the first of the sulfonylureas in 1942
- Reintroduction of the use of biguanides for Type 2 diabetes in the late 1950s. The initial phenformin was withdrawn worldwide (in the U.S. in 1977) due to its potential for sometimes fatal lactic acidosis and metformin was first marketed in France in 1979, but not until 1994 in the US.
- The determination of the amino acid sequence of insulin (by Sir Frederick Sanger, for which he received a Nobel Prize)
- The radioimmunoassay for insulin, as discovered by Rosalyn Yalow and Solomon Berson (gaining Yalow the 1977 Nobel Prize in Physiology or Medicine)
- The three-dimensional structure of insulin (PDB 2INS)
- Dr Gerald Reaven's identification of the constellation of symptoms now called metabolic syndrome in 1988
- Demonstration that intensive glycemic control in type 1 diabetes reduces chronic side effects more as glucose levels approach 'normal' in a large longitudinal study, and also in type 2 diabetics in other large studies
- Identification of the first thiazolidinedione as an effective insulin sensitizer during the 1990s
In 1980, U.S. biotech company Genentech developed human insulin. The insulin is isolated from genetically altered bacteria (the bacteria contain the human gene for synthesizing human insulin), which produce large quantities of insulin. Scientists then purify the insulin and distribute it to pharmacies for use by diabetes patients.
Social issues
The 1990 "St Vincent Declaration" was the result of international efforts to improve the care accorded to those with diabetes. Doing so is important both in terms of quality of life and life expectancy but also economically-expenses due to diabetes have been shown to be a major drain on health-and productivity-related resources for healthcare systems and governments.
Several countries established more and less successful national diabetes programmes to improve treatment of the disease.
A study shows that diabetic patients with neuropathic symptoms such as numbness or tingling in feet or hands are twice as likely to be unemployed as those without the symptoms.
referances:
Wikipedia, the free encyclopedia
American Diabetes Association
http://diabetes.webmed.com
www.medicinenet.com
http://www.cdc.gov/diabetes
|